Preventing infectious diseases
Preventing infectious diseases is a paramount concern in public health. It involves a multifaceted approach aimed at reducing the transmission and impact of diseases that can easily spread from person to person. This includes promoting vaccination programs to bolster immunity, practicing good hygiene like regular handwashing, maintaining proper sanitation to limit disease vectors, and implementing quarantine measures when necessary. Education and awareness campaigns play a vital role in encouraging individuals and communities to adopt these preventive measures. Moreover, timely and effective responses to outbreaks and global cooperation are essential components of a robust strategy to combat the spread of infectious diseases, safeguarding the well-being of populations worldwide.

With the continuous increase in global connectivity and the rapid movement of individuals and goods across borders, infectious diseases have become an increasingly vital health challenge in the modern age. Preventing infectious diseases has become a critical issue for public health, requiring comprehensive strategies and collective efforts from individuals, communities, and healthcare institutions alike. Prevention aims to reduce the transmission and control of these diseases by promoting awareness and implementing appropriate preventive measures. In this context, we will explore the importance of immunizations, personal hygiene practices, maintaining public sanitation, and following health safety guidelines during outbreaks.
The Importance of Preventing Infectious Diseases
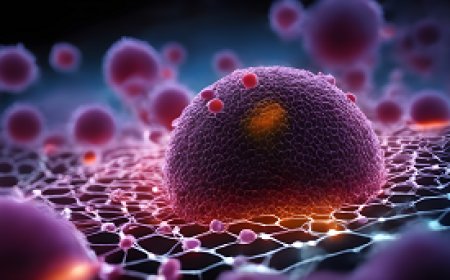
Disease prevention is a critical aspect of public health, and it plays a fundamental role in reducing the burden of infectious diseases on individuals and society as a whole. Infectious diseases are caused by microorganisms such as bacteria, viruses, fungi, and parasites, and they can be transmitted from person to person or through contact with contaminated surfaces, food, or water.
Preventing infectious diseases is of paramount importance for several reasons.
-
Reducing the Burden on Healthcare Systems: When infectious diseases spread uncontrollably, they can lead to epidemics or pandemics, overwhelming healthcare systems. The strain on medical facilities, personnel, and resources can result in a shortage of care for not only those affected by the infectious disease but also for those with other health conditions.
-
Protecting Vulnerable Populations: Certain individuals, such as the elderly, infants, and people with weakened immune systems, are more susceptible to severe infections. By preventing infectious diseases, we protect these vulnerable populations who are at a higher risk of complications or death.
-
Preventing Unnecessary Deaths: Infectious diseases are responsible for a significant number of preventable deaths worldwide. Disease prevention measures, such as vaccination and hygiene practices, can save countless lives by reducing the spread of these diseases.
-
Preserving Quality of Life: Many infectious diseases can have long-lasting or debilitating effects on those who survive them. For example, polio can cause permanent paralysis, and hepatitis can lead to liver damage. Preventing these diseases preserves the quality of life for individuals and their families.
-
Economic Impact: Infectious diseases have a substantial economic impact. They result in lost productivity due to illness and, in some cases, can disrupt trade and travel. Investments in disease prevention can yield significant returns by reducing the economic burden of illness.
-
Global Health Security: In a globalized world, infectious diseases can easily cross borders. Preventing infectious diseases is not only a matter of local concern but also a global one. Disease prevention contributes to global health security, preventing the international spread of diseases and the potential for pandemics.
-
Preservation of Antibiotics: Overuse and misuse of antibiotics have led to the development of antibiotic-resistant strains of bacteria, often referred to as superbugs. Preventing infectious diseases, where possible, reduces the need for antibiotics and helps to preserve these critical drugs for cases where they are truly needed.
-
Promoting Health Equity: Access to disease prevention measures such as vaccines, clean water, and sanitation is an essential component of health equity. Disease prevention efforts can help reduce health disparities among different populations and communities.
-
Personal and Community Well-being: Disease prevention measures like vaccination, handwashing, and safe food handling not only protect individuals but also contribute to the well-being of the entire community. High vaccination rates, for instance, create herd immunity, which offers protection to those who cannot be vaccinated.
-
Environmental Impact: Many infectious diseases, such as those transmitted by water or vectors like mosquitoes, are closely tied to environmental conditions. By preventing these diseases, we can also work to protect and preserve the environment.
the importance of preventing infectious diseases cannot be overstated. Disease prevention measures, including vaccinations, education, sanitation, and good hygiene practices, are vital in safeguarding public health, reducing the burden on healthcare systems, and promoting a healthier, more productive, and equitable society. A concerted effort at all levels of society, from individual actions to international cooperation, is necessary to effectively prevent and control infectious diseases.
Vaccination: A Key Tool in Disease Prevention
Disease prevention is at the forefront of public health initiatives, and vaccination stands out as one of the most effective and essential tools in this endeavor. Vaccines have played a critical role in preventing infectious diseases, reducing their impact on individuals, communities, and the global population. Here, we'll delve into the importance of vaccination in disease prevention.
1. Disease Eradication:
Vaccination has been instrumental in the eradication of some of the most deadly and debilitating diseases in history. Perhaps the most notable example is the smallpox vaccine, which led to the complete eradication of the smallpox virus. This success demonstrates the extraordinary power of vaccines in disease prevention.
2. Herd Immunity:
One of the key benefits of vaccination is the establishment of herd immunity. When a significant portion of a population is immunized against a specific disease, it becomes challenging for the disease to spread within the community. This indirectly protects those who cannot be vaccinated, such as individuals with certain medical conditions or allergies.
3. Prevention of Outbreaks:
Vaccination programs have been crucial in preventing disease outbreaks. Measles, mumps, and pertussis (whooping cough) are examples of vaccine-preventable diseases that can spread rapidly and cause outbreaks in unvaccinated or under-vaccinated populations. By achieving high vaccination rates, these outbreaks can be prevented.
4. Reducing Severity and Complications:
Even when vaccines don't entirely prevent infections, they often reduce the severity of the disease and its associated complications. For instance, the flu vaccine may not prevent all cases of the flu, but it significantly decreases the risk of severe illness, hospitalization, and death.
5. Saving Lives:
Vaccination saves lives. Diseases like polio, diphtheria, and tetanus, which were once common causes of death, have become rare due to vaccination. By preventing these diseases, vaccines have directly saved countless lives.
6. Cost-Effective Public Health Strategy:
Vaccination is a cost-effective public health strategy. It is often more economical to prevent diseases through vaccination than to treat them once they have already spread. Vaccination programs save healthcare costs and resources.
7. Shielding Vulnerable Populations:
Many individuals, such as the very young, the elderly, and those with compromised immune systems, are particularly susceptible to infectious diseases. Vaccination not only protects these vulnerable groups but also helps create a protective barrier in the community.
8. Global Disease Control:
Vaccination is an integral part of global disease control efforts. International vaccination campaigns have helped prevent the spread of diseases across borders and contributed to the control of pandemics, such as the H1N1 influenza pandemic in 2009.
9. Scientific Advancements:
Advances in vaccine technology have made it possible to develop vaccines more rapidly and effectively. This is particularly crucial in responding to emerging infectious diseases and evolving pathogens, as demonstrated during the COVID-19 pandemic.
10. Building a Healthier Future:
Vaccination is not just about preventing diseases in the present; it's about building a healthier future. By ensuring that future generations are protected from infectious diseases, we contribute to long-term disease prevention and overall well-being.
vaccination is a cornerstone of disease prevention, and its impact on public health cannot be overstated. It has a profound role in controlling and preventing the spread of infectious diseases, reducing the severity of illnesses, saving lives, and building healthier, more resilient communities. Comprehensive vaccination programs, public education, and equitable access to vaccines are essential components of global efforts to prevent the spread of diseases and protect public health.
Hand Hygiene and Its Role in Infection Control
Hand hygiene is a fundamental practice in infection control and plays a pivotal role in preventing the spread of infectious diseases. Whether in healthcare settings, public spaces, or daily life, maintaining proper hand hygiene is essential for disease prevention.
The importance of hand hygiene in controlling infections and ultimately safeguarding public health.
1. Disease Transmission through Hands: Our hands are one of the most common vectors for disease transmission. They come into contact with various surfaces, objects, and people, making them potential carriers of harmful microorganisms. Touching contaminated surfaces and then the face, eyes, nose, or mouth can introduce pathogens into the body.
2. Importance in Healthcare Settings: Hand hygiene is paramount in healthcare facilities. Healthcare workers who don't adhere to strict hand hygiene protocols can inadvertently transmit infections to patients and colleagues. Infection control measures, including handwashing and hand sanitization, are crucial in preventing healthcare-associated infections (HAIs).
3. Prevention of Common Infections: Hand hygiene is effective in preventing common infectious diseases like the flu, colds, and gastrointestinal illnesses. These diseases often spread through contact with contaminated hands, especially in crowded environments.
4. Reducing Antibiotic Resistance: Proper hand hygiene can help reduce the need for antibiotics. When infections are prevented through good hand hygiene practices, the overuse and misuse of antibiotics can be minimized. This, in turn, helps combat the global issue of antibiotic resistance.
5. Protection of Vulnerable Populations: Vulnerable populations, including the elderly, young children, and individuals with weakened immune systems, are at higher risk of severe infections. Maintaining good hand hygiene helps protect these at-risk groups from potentially life-threatening illnesses.
6. Role in Pandemic Control: During pandemics, such as the COVID-19 pandemic, hand hygiene has been a key component of infection control strategies. Regular handwashing and the use of hand sanitizers have been widely promoted to reduce the spread of the virus.
7. Handwashing Technique: Proper handwashing involves using soap and water, rubbing hands together for at least 20 seconds, cleaning all hand surfaces, and rinsing thoroughly. Hand sanitizers with at least 60% alcohol content are an effective alternative when soap and water are not readily available.
8. Hand Hygiene in Public Spaces: Beyond healthcare settings, good hand hygiene in public spaces is crucial. Providing access to hand sanitizers and promoting handwashing in schools, workplaces, public transportation, and recreational facilities can significantly reduce the risk of disease transmission.
9. Behavior Change and Education: Public health campaigns and educational programs play a vital role in promoting hand hygiene. Teaching individuals about the importance of hand hygiene, proper techniques, and when to wash their hands is essential for creating lasting behavior change.
10. Personal Responsibility: Ultimately, maintaining good hand hygiene is a personal responsibility. Each individual can contribute to disease prevention by practicing regular handwashing and sanitizing, especially after being in public places, before eating, and after coughing or sneezing.
hand hygiene is a cornerstone of infection control and a powerful tool for disease prevention. It is essential in healthcare settings to protect patients and healthcare workers, but it is also vital in everyday life to reduce the risk of common infections and contribute to public health. Comprehensive hand hygiene practices, along with public education and the promotion of personal responsibility, are critical components of efforts to control infectious diseases and prevent their spread.
Maintaining Clean Environments to Prevent Disease Spread
Disease prevention is a top priority in public health, and one of the most effective strategies is the maintenance of clean environments. Clean environments play a pivotal role in preventing the spread of infectious diseases. Whether in healthcare facilities, homes, schools, workplaces, or public spaces, cleanliness is essential for disease prevention. This article delves into the significance of maintaining clean environments in controlling infections and safeguarding public health.
1. Contaminant Removal:
Clean environments help in the removal of contaminants and pathogens that can cause diseases. Regular cleaning practices, such as dusting, sweeping, and disinfecting surfaces, minimize the presence of disease-causing agents.
2. Reducing Disease Transmission:
Pathogens and infectious agents often reside on surfaces and objects. When these surfaces are clean, the risk of disease transmission through contact is significantly reduced. Clean hands, clean surfaces, and clean air contribute to a healthier environment.
3. Healthcare Settings:
In healthcare facilities, maintaining a clean and sterile environment is crucial for preventing healthcare-associated infections (HAIs). Regular cleaning and sterilization of medical equipment, surfaces, and patient rooms help protect both patients and healthcare workers.
4. Preventing Common Infections:
In everyday life, maintaining cleanliness is essential for preventing common infections like colds, flu, and gastrointestinal diseases. These diseases can easily spread in unsanitary environments.
5. Food Safety:
Clean environments are vital for food safety. Inadequate food hygiene can lead to foodborne illnesses. Proper food handling, storage, and kitchen cleanliness can prevent the contamination of food and the spread of diseases.
6. Hygiene Education:
Educating individuals about the importance of maintaining clean environments is crucial for promoting good hygiene practices. This education can help people understand the connection between cleanliness and disease prevention.
7. Personal Responsibility:
Each individual shares the responsibility for maintaining a clean environment. Practicing personal hygiene, such as regular handwashing, proper waste disposal, and cleaning personal spaces, is essential for preventing disease transmission.
8. Air Quality:
Air quality is a crucial aspect of a clean environment. Proper ventilation and air filtration systems help remove airborne pathogens and maintain a healthy indoor environment. This is especially important in reducing the risk of respiratory infections.
9. Reducing the Environmental Reservoir:
Clean environments help reduce the environmental reservoir of infectious agents. For example, stagnant water and uncleaned surfaces can become breeding grounds for disease vectors like mosquitoes, leading to diseases such as malaria and dengue fever.
10. Crisis Preparedness:
Maintaining clean environments is vital during public health crises, such as pandemics. Regular cleaning and disinfection of public spaces, including public transportation, can help reduce the spread of infectious diseases.
11. Sustainable Disease Prevention:
Clean environments are crucial for long-term, sustainable disease prevention. Public health measures like vaccination and treatment are important, but cleanliness and hygiene are the foundation for preventing the emergence and spread of infectious diseases.
maintaining clean environments is an essential aspect of disease prevention. Cleanliness is not limited to hospitals but extends to our homes, schools, workplaces, and public spaces. It is integral to reducing the transmission of infectious diseases, safeguarding public health, and building resilient, disease-resistant communities. Comprehensive public health strategies, education, and personal responsibility all contribute to the maintenance of clean environments as a means of disease prevention.
Quarantine and Isolation Measures in Epidemic Management
In the field of disease prevention, particularly during epidemics and pandemics, quarantine and isolation measures are crucial tools for controlling the spread of infectious diseases. These strategies help limit the transmission of pathogens, safeguard public health, and mitigate the impact of outbreaks. This article explores the importance and implementation of quarantine and isolation in epidemic management and disease prevention.
1. Distinction between Quarantine and Isolation:
- Quarantine: Quarantine is the practice of separating and restricting the movement of individuals who may have been exposed to a contagious disease but are not yet showing symptoms. It is a preventive measure to monitor and prevent the potential spread of the disease.
- Isolation: Isolation involves separating infected individuals from those who are not infected. It is applied to individuals who are confirmed to have a contagious disease to prevent its spread to others.
2. Early Detection and Containment:
Quarantine and isolation are vital for early detection and containment of infectious diseases. By isolating or quarantining individuals who are potentially infected or already infected, public health authorities can prevent the further spread of the disease within communities.
3. Minimizing Community Transmission:
These measures help in minimizing community transmission of diseases, especially when dealing with highly contagious pathogens such as the novel coronavirus (SARS-CoV-2). By restricting the movement of infected or exposed individuals, the likelihood of new cases is reduced.
4. Protecting Vulnerable Populations:
Quarantine and isolation protect vulnerable populations, including the elderly and those with pre-existing health conditions, who are at a higher risk of severe illness or death from infectious diseases.
5. Preventing Healthcare System Overwhelm:
By limiting the number of individuals requiring medical care, quarantine and isolation measures prevent overwhelming healthcare systems during epidemics. This ensures that hospitals can provide adequate care to those in need.
6. Contact Tracing:
Quarantine and isolation are closely linked to contact tracing. When an individual is confirmed to have an infectious disease, contact tracing is conducted to identify and notify individuals who may have been exposed. These contacts are then placed in quarantine to prevent further transmission.
7. Legal and Ethical Considerations:
Implementing quarantine and isolation measures involves complex legal and ethical considerations. Balancing public health with individual rights and privacy is a challenge that health authorities must navigate carefully.
8. Public Compliance and Education:
The success of quarantine and isolation measures relies on public compliance and education. Public health campaigns and clear communication are crucial to inform the public about the importance of these measures and how to follow them correctly.
9. Duration of Quarantine and Isolation:
The duration of quarantine and isolation varies depending on the disease and guidelines provided by health authorities. It is typically based on the incubation period of the disease and the time it takes for an individual to become non-infectious.
10. Monitoring and Support:
Those under quarantine or isolation require monitoring of their health status. They may also need support, such as access to medical care, mental health services, and provisions for basic needs.
11. Exit Strategies:
Developing exit strategies is essential to ensure that individuals can safely reintegrate into society once they are no longer a risk of transmitting the disease. This involves a clear assessment of the individual's health and the testing and clearance process.
quarantine and isolation measures are indispensable tools in epidemic management and disease prevention. They serve as a first line of defense against the spread of infectious diseases, protecting individuals and communities. Proper implementation, public cooperation, and ethical considerations are essential for their success. Public health authorities must strike a balance between safeguarding public health and respecting individual rights, all while focusing on reducing the impact of epidemics on society.
Public Awareness and Education in Disease Prevention
Public awareness and education play a critical role in disease prevention. Informed and educated communities are better equipped to understand, respond to, and actively participate in efforts to prevent the spread of infectious diseases. This article explores the importance of public awareness and education in disease prevention and the various ways in which they can be effectively implemented.
1. Knowledge is Power:
- When the public is informed about infectious diseases, their modes of transmission, and prevention strategies, they are more likely to make informed decisions about their health and engage in preventive behaviors.
- Education empowers individuals to take personal responsibility for their health and the health of their communities.
2. Early Detection and Reporting:
- Educated individuals are more likely to recognize the early signs and symptoms of diseases. This early detection can lead to quicker medical intervention and containment efforts.
- Encouraging the public to report symptoms and seek medical attention when needed is vital in the early stages of an outbreak.
3. Promoting Vaccination:
- Public education is essential in dispelling myths and misconceptions about vaccines. When the community understands the safety and effectiveness of vaccines, vaccination rates increase, leading to herd immunity.
- Herd immunity helps protect vulnerable populations who cannot receive vaccinations, such as individuals with certain medical conditions.
4. Behavior Change:
- Education can drive behavior change. It can encourage individuals to adopt healthier practices like regular handwashing, practicing safe sex, and adopting a balanced diet.
- Information campaigns can motivate individuals to engage in protective behaviors, such as using condoms to prevent the spread of sexually transmitted infections.
5. Reducing Stigma:
- Public education can help reduce the stigma associated with infectious diseases. Stigmatizing attitudes can discourage individuals from seeking testing and treatment, thus perpetuating the spread of diseases.
- Understanding the science behind diseases can reduce fear and discrimination.
6. Preparedness and Response:
- An informed public is better prepared to respond to outbreaks and follow public health guidelines. They are more likely to cooperate with quarantine and isolation measures when they understand their purpose.
- Education can help the public understand the importance of social distancing, mask-wearing, and other preventive measures during epidemics.
7. Targeted Messaging:
- Tailored messages for different populations are important. For example, educating school children about good hygiene practices can prevent the spread of illnesses in schools, while providing parents with information about vaccination schedules is crucial.
- Messages should be clear, culturally sensitive, and accessible to diverse groups.
8. Media and Technology:
- The media, including social media, can be powerful tools for disseminating information. Public health authorities can use these channels to reach a wide audience quickly.
- Educational campaigns should also address misinformation and provide credible sources of information to combat the spread of false or misleading information.
9. Community Engagement:
- Engaging communities in educational efforts fosters a sense of ownership and responsibility. Community leaders, schools, and local organizations can all play a role in disseminating information.
- Public participation in health initiatives strengthens collective efforts in disease prevention.
10. Long-Term Benefits:
- Public awareness and education have long-term benefits. Informed communities are better prepared for future health crises and more likely to adopt a culture of health-conscious behaviors.
- Investing in public health education is an investment in the resilience of a society.
public awareness and education are fundamental components of disease prevention. Informed communities are more likely to adopt healthier practices, respond effectively to outbreaks, and reduce the stigma associated with infectious diseases. Public health authorities, community organizations, and educational institutions must work together to ensure that information is accurate, accessible, and culturally sensitive. Disease prevention is not only a matter of medical interventions but also of education and empowerment at the community level.
Global Cooperation in Combating Infectious Diseases
In an interconnected world, where people and goods move across borders with unprecedented ease, global cooperation is essential in combating infectious diseases. Disease prevention on a global scale is a collective effort that requires the collaboration of countries, international organizations, healthcare professionals, and the public. This article delves into the significance of global cooperation in combating infectious diseases and its role in disease prevention.
1. Early Warning and Surveillance:
- Global cooperation enables the sharing of information and data related to disease outbreaks. Through organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), countries can provide early warnings about potential epidemics.
- Surveillance systems help track the spread of diseases, assess their severity, and facilitate timely response efforts.
2. Rapid Response and Resource Allocation:
- When an infectious disease emerges, a coordinated global response can quickly mobilize resources, medical personnel, and supplies to affected areas. This helps contain the disease and prevent it from spreading.
- Countries can benefit from resource-sharing agreements during crises, such as access to vaccines or medical equipment.
3. Research and Vaccine Development:
- Global cooperation fosters collaborative research efforts. Scientists and researchers from around the world can pool their expertise to better understand the pathogens causing diseases and develop vaccines.
- Initiatives like COVAX aim to ensure equitable access to vaccines during pandemics, recognizing that a global approach is vital in vaccine distribution.
4. Information Sharing and Best Practices:
- Sharing information about effective disease prevention strategies and best practices is crucial. Countries can learn from each other's successes and challenges in managing outbreaks.
- Learning from past experiences can help countries adapt their response strategies to be more effective in the future.
5. Capacity Building and Training:
- Developing countries often lack the resources and expertise to respond effectively to infectious diseases. Global cooperation involves capacity building, which includes training healthcare workers, strengthening healthcare systems, and improving laboratory capabilities.
- These efforts not only benefit the countries directly involved but also enhance global preparedness.
6. Travel Restrictions and Border Control:
- During a disease outbreak, countries may implement travel restrictions and border control measures. However, these should be coordinated globally to avoid negative economic and social impacts.
- Collaboration can help establish guidelines for travel restrictions that are based on scientific evidence and consider the free flow of essential goods and services.
7. Pandemic Preparedness:
- Global cooperation extends to pandemic preparedness, which involves planning, simulation exercises, and stockpiling of essential medical supplies. The objective is to be ready for future outbreaks.
- The Pandemic Influenza Preparedness Framework, for example, aims to enhance global preparedness for influenza pandemics.
8. Ethical Considerations:
- Ethical concerns related to research, vaccine distribution, and the sharing of medical supplies must be addressed through global cooperation. Fair and equitable access to resources is crucial.
- Ensuring that the benefits of research and medical advancements are distributed fairly is a shared responsibility.
9. Public Awareness and Behavior:
- Public awareness campaigns about infectious diseases should be coordinated globally to ensure consistent and accurate information reaches the public. Misinformation and panic can be detrimental.
- Encouraging behavior that supports disease prevention, such as mask-wearing and vaccination, should be a global effort.
10. Long-Term Investments:
- Global cooperation in combating infectious diseases is a long-term investment in global health security. The cost of responding to pandemics far exceeds the cost of prevention and preparedness.
- The world must recognize the importance of sustained commitment to disease prevention to mitigate future global health crises.
global cooperation in combating infectious diseases is not a choice but a necessity. In a world where borders are porous and diseases recognize no boundaries, collaborative efforts are crucial for disease prevention and control. The recent COVID-19 pandemic serves as a stark reminder of the importance of a united global response. While challenges exist, such as political tensions and resource disparities, they must be overcome for the sake of global health and well-being.
Emerging Infectious Diseases: Challenges and Preparedness
Emerging infectious diseases (EIDs) pose a constant threat to global public health. These diseases, which are caused by newly identified pathogens or known pathogens that have evolved, present unique challenges in terms of prevention, containment, and management. In this article, we will explore the challenges associated with emerging infectious diseases and the importance of preparedness in preventing their spread.
Challenges of Emerging Infectious Diseases:
-
Unpredictability: One of the major challenges of EIDs is their unpredictability. New diseases can arise suddenly, and it can be difficult to anticipate when and where they will emerge. This unpredictability can lead to delayed responses, allowing diseases to spread.
-
Globalization: In today's highly interconnected world, diseases can travel rapidly across borders. International travel and trade can facilitate the rapid spread of infectious agents, making it challenging to contain outbreaks.
-
Environmental Factors: Environmental changes, such as deforestation and climate change, can alter the distribution of disease vectors like mosquitoes and promote the emergence of new diseases. These changes can also affect the habitats of reservoir hosts, which may carry diseases.
-
Antimicrobial Resistance: The emergence of drug-resistant strains of pathogens complicates the treatment of infectious diseases. Antibiotics and antiviral drugs may become less effective, making it harder to control outbreaks.
-
Vaccine Development: Developing vaccines for newly emerging diseases can be a lengthy and complex process. The time it takes to research, develop, test, and produce a vaccine can hinder rapid disease prevention efforts.
Preparedness for Emerging Infectious Diseases:
-
Surveillance and Early Warning Systems: A robust global surveillance system is crucial for the early detection of EIDs. Timely identification and reporting of outbreaks are essential for initiating containment measures.
-
Research and Development: Governments, international organizations, and the private sector should invest in research and development to create rapid diagnostic tools, treatments, and vaccines. This requires a coordinated effort to shorten the time it takes to respond to new diseases.
-
Capacity Building: Countries, especially those with weaker healthcare systems, need to build their capacity for disease detection, response, and research. Training healthcare workers, strengthening laboratory networks, and enhancing healthcare infrastructure are vital components of preparedness.
-
Global Coordination: International cooperation is paramount. This involves sharing data, resources, and expertise. Initiatives like the Global Outbreak Alert and Response Network (GOARN) facilitate global collaboration during outbreaks.
-
Community Engagement: Involving local communities in disease prevention and response efforts is essential. Communities can serve as the first line of defense by reporting outbreaks and practicing preventive measures.
-
Regulatory Frameworks: International agreements and regulatory frameworks can expedite the development and distribution of vaccines and treatments. The Pandemic Influenza Preparedness Framework, for example, helps ensure equitable access to vaccines during pandemics.
-
Ethical Considerations: Ethical principles must guide all actions related to EIDs, including research, vaccine distribution, and resource allocation. Fair and equitable access to resources and benefits should be a priority.
-
Education and Public Awareness: Raising awareness about EIDs and promoting good hygiene and preventive behaviors is crucial. Education empowers individuals to take personal responsibility for their health and adopt disease prevention measures.
-
Stockpiling Resources: Maintaining stockpiles of essential medical supplies, such as personal protective equipment and antiviral drugs, can help ensure that countries are well-prepared to respond to outbreaks.
-
Flexible Response Strategies: Preparedness plans should be adaptable to different scenarios. The ability to scale up or down response efforts based on the severity of the outbreak is vital.
emerging infectious diseases are a persistent global challenge. Their unpredictability and potential for rapid spread make preparedness and global cooperation essential for effective disease prevention. Investing in research, surveillance, and healthcare infrastructure, along with ethical considerations and community engagement, are key components of a comprehensive approach to addressing these challenges. By working together and remaining vigilant, the global community can better prepare for and respond to emerging infectious diseases and ultimately prevent their devastating impact.
The Role of Healthcare Workers in Disease Prevention
Healthcare workers play a pivotal role in disease prevention. They are on the front lines of patient care and have a significant impact on controlling the spread of infectious diseases. This role becomes even more critical during outbreaks and pandemics, as healthcare workers are at the forefront of diagnosis, treatment, and containment efforts. In this article, we will delve into the various aspects of the role of healthcare workers in disease prevention.
1. Patient Care and Education:
Healthcare workers are responsible for providing care to patients, which includes diagnosing and treating diseases. They have the expertise to identify symptoms and risk factors and can provide guidance on preventive measures. Educating patients about hygiene practices, vaccination, and other preventive strategies is an essential part of their role.
2. Infection Control:
Healthcare workers are trained in infection control measures to minimize the risk of transmitting diseases within healthcare settings. They ensure that proper hand hygiene, personal protective equipment, and disinfection protocols are followed rigorously to protect both patients and themselves.
3. Vaccination:
Healthcare workers are often involved in administering vaccines. They not only administer routine vaccines but also play a crucial role in mass vaccination campaigns during outbreaks. By ensuring high vaccination coverage, they contribute to herd immunity, which prevents the spread of diseases within communities.
4. Surveillance and Reporting:
Healthcare workers are responsible for monitoring and reporting notifiable diseases. They play a key role in early detection and response to outbreaks. Reporting cases to public health authorities is essential for timely intervention and disease prevention.
5. Quarantine and Isolation:
During outbreaks, healthcare workers are involved in implementing quarantine and isolation measures to prevent the spread of diseases. They decide when and how individuals should be isolated or quarantined, reducing the risk of transmission.
6. Contact Tracing:
Contact tracing is crucial in identifying and notifying individuals who may have been exposed to infectious diseases. Healthcare workers play a central role in this process by tracking down and informing potential contacts, thus preventing further transmission.
7. Research and Development:
Healthcare workers often engage in clinical research and contribute to the development of new treatments and vaccines. Their insights and expertise help advance medical science, ultimately leading to better disease prevention and management strategies.
8. Preparedness and Training:
In the face of emerging infectious diseases, healthcare workers must be well-prepared. Regular training in outbreak response and emergency preparedness equips them with the skills and knowledge needed to act swiftly during disease outbreaks.
9. Public Awareness and Advocacy:
Healthcare workers are in a unique position to raise public awareness about disease prevention. Through public health campaigns and advocacy, they can promote health behaviors, encourage vaccination, and dispel misinformation.
10. Ethical Considerations:
Healthcare workers must adhere to ethical principles in their practice. This includes respecting patient autonomy, ensuring confidentiality, and making decisions that prioritize the welfare of patients while considering the greater public good.
11. Personal Health and Well-being:
Healthcare workers must take care of their own health and well-being to continue their essential work. Ensuring that they are immunized, follow safety guidelines, and manage stress is vital for their own health and preventing the transmission of diseases within healthcare settings.
12. Research and Learning:
Healthcare workers should continuously engage in professional development and stay up to date with the latest developments in disease prevention and treatment. This lifelong learning ensures that they provide the best possible care and advice to patients.
healthcare workers are the linchpin of disease prevention. Their roles encompass a wide range of activities, from direct patient care to public health advocacy and research. Their expertise and dedication are critical in controlling the spread of infectious diseases, and they play a central role in safeguarding public health, particularly during disease outbreaks and pandemics. Disease prevention relies heavily on the knowledge, skills, and commitment of healthcare workers who work tirelessly to protect the health and well-being of individuals and communities.
Innovations in Pandemic Preparedness and Response
Pandemics represent a significant threat to global public health and can have devastating consequences for societies, economies, and healthcare systems. The COVID-19 pandemic, which began in late 2019, serves as a stark reminder of the importance of being prepared to prevent and respond to infectious diseases on a global scale. To effectively combat pandemics, continuous innovation is crucial in the realm of preparedness and response. This article explores various innovations in pandemic preparedness and response with a focus on disease prevention.
1. Surveillance and Early Warning Systems:
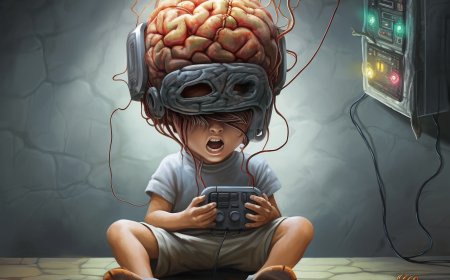
Advanced surveillance and early warning systems are pivotal in detecting and responding to potential pandemics. Innovations in data analytics, artificial intelligence (AI), and machine learning have enabled the rapid analysis of large datasets to identify unusual patterns of disease and predict outbreaks. Mobile health apps and wearable devices can track individuals' health, helping to detect early symptoms or unusual trends in specific regions.
2. Diagnostic Tools and Testing Innovations:
Rapid and accurate diagnostic tests are fundamental to disease prevention and control. Innovations in diagnostic technologies have led to the development of point-of-care testing devices, such as rapid antigen tests and PCR machines. These innovations have made it possible to quickly identify infected individuals, isolate them, and implement contact tracing to prevent further transmission.
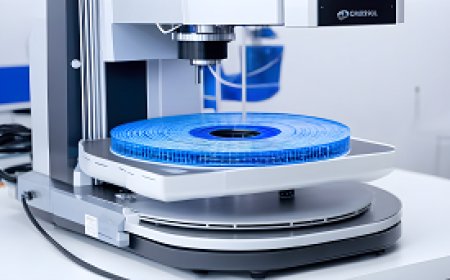
3. Vaccine Development and Distribution:
Vaccines are a cornerstone of pandemic prevention. Advances in vaccine technology, like messenger RNA (mRNA) vaccines, have revolutionized the speed at which vaccines can be developed and produced. Moreover, innovations in cold-chain logistics and distribution networks ensure vaccines reach remote and vulnerable populations.
4. Telemedicine and Remote Care:
Telemedicine and remote healthcare platforms have gained prominence during pandemics. These innovations allow individuals to consult healthcare professionals without physical contact, reducing the risk of disease transmission. Telemedicine also helps manage and monitor patients remotely, freeing up healthcare facilities for critical cases.
5. Contactless Technologies:
The use of contactless technologies in various settings, from touchless payment systems to automated check-ins at healthcare facilities, has become essential for reducing the spread of infectious diseases. These innovations minimize physical interactions and reduce the risk of fomite transmission.
6. Personal Protective Equipment (PPE) Innovations:
Innovations in PPE design and materials have improved the safety and comfort of frontline healthcare workers. This includes the development of reusable, durable, and more effective protective gear, as well as advanced ventilation systems in healthcare settings.
7. Tele-Education and Training:
The training of healthcare workers and the public has been transformed through tele-education. Virtual platforms enable the dissemination of information, guidelines, and best practices rapidly. Simulation-based training, augmented reality, and virtual reality have become valuable tools in preparing healthcare workers for pandemic scenarios.
8. Public Health Messaging and Behavioral Insights:
Innovations in public health messaging and the use of behavioral insights have been critical in encouraging preventive behaviors, such as mask-wearing, hand hygiene, and social distancing. Digital communication channels and social media analytics help tailor messages to specific demographics and cultures.
9. Genomic Sequencing and Tracking Variants:
Genomic sequencing plays a vital role in monitoring the evolution of pathogens and tracking variants that may impact disease transmission or vaccine effectiveness. Innovations in high-throughput sequencing technologies have accelerated our understanding of emerging diseases.
10. Artificial Intelligence in Drug Discovery:
Artificial intelligence has transformed drug discovery processes, speeding up the identification of potential treatments. Machine learning algorithms can analyze vast databases to identify existing drugs that may be repurposed to combat new diseases.
11. Community Engagement and Local Initiatives:
Innovations in community engagement have empowered local initiatives to prevent the spread of diseases. Communities have used digital platforms to share information, coordinate resources, and support vulnerable members.
12. Supply Chain Resilience:
Ensuring the resilience of supply chains for medical equipment, pharmaceuticals, and other essential supplies is crucial. Innovations in supply chain management and distribution logistics are enhancing the availability of critical resources during pandemics.
innovations in pandemic preparedness and response are essential in the ongoing battle against infectious diseases. These innovations encompass a wide range of fields, from advanced technologies like AI and genomics to practical solutions such as contactless technologies and telemedicine. As the world faces new and evolving threats from infectious diseases, the ability to adapt and innovate will be a key factor in disease prevention and control. It is crucial that governments, healthcare institutions, researchers, and the private sector continue to invest in and embrace these innovations to build a safer and more prepared world.
In conclusion
it is important to recognize that preventing infectious diseases is a collective effort to safeguard public health and ensure the safety of communities. These efforts rely on awareness and collaboration among individuals, healthcare institutions, and governments. Investing in prevention yields significant benefits by reducing the spread of diseases and alleviating health and economic burdens.
Both at the national and international levels, the prevention of infectious diseases should be at the forefront of the health agenda, with a focus on research and innovation in this field. It requires cooperation between nations, continuous information exchange, and resource sharing to combat diseases on a global scale.
In short, preventing infectious diseases is an investment in the future and an opportunity to protect public health and elevate human life. Adopting a healthy lifestyle and adhering to preventive guidelines promote health sustainability, improving the quality of our lives and our well-being.
What's Your Reaction?