Artificial Intelligence in Medicine: The Future of Healthcare
Artificial intelligence in healthcare is an exciting application that represents the future of healthcare. AI allows doctors and nurses to have a better understanding of diagnoses and treatments through the analysis of big data and machine learning. Robots and automation can be used to enhance healthcare efficiency and improve patient experiences. It can be said that artificial intelligence paves the way for a promising future where better and more accurate healthcare can be delivered.

In the era of rapid technological innovation, artificial intelligence stands as a key to the future of healthcare. The alliance between the fields of medicine and artificial intelligence is on the brink of a radical transformation in how healthcare is delivered and diseases are diagnosed. Artificial intelligence enables healthcare professionals to improve diagnostic accuracy and provide better treatments by analyzing vast amounts of data and utilizing machine learning. Furthermore, robots and automation can be employed to enhance healthcare efficiency and improve the patient experience. In this introduction, we will explore how artificial intelligence shapes the future of healthcare, enhancing the quality of medical services while considering the concept of medicine and artificial intelligence.
AI for Disease Diagnosis
The intersection of medicine and artificial intelligence (AI) has given rise to a promising field: AI for disease diagnosis. In this incredibly dull discussion, we will delve into the intricacies of how AI is transforming the landscape of medical diagnosis.
1. Data Collection and Integration:
AI for disease diagnosis heavily relies on data, and in the medical field, data comes from various sources such as electronic health records, medical imaging, and patient histories. Integrating and structuring this data is the initial challenge. AI systems must collect, aggregate, and make sense of diverse data formats to support accurate diagnosis.
2. Image Analysis:
Medical imaging is a fundamental aspect of disease diagnosis. AI algorithms can analyze medical images such as X-rays, MRIs, and CT scans with remarkable precision. These algorithms identify anomalies, detect patterns, and provide insights to healthcare professionals, contributing to early and accurate diagnoses.
3. Natural Language Processing (NLP):
NLP plays a critical role in analyzing unstructured data in medical records, research papers, and clinical notes. AI-driven NLP systems extract valuable information, helping doctors make informed decisions based on textual data.
4. Machine Learning and Deep Learning:
Machine learning and deep learning techniques enable AI systems to learn from large datasets. They can identify trends and correlations that might be too subtle for human detection. These algorithms improve diagnostic accuracy and support predictive analysis.
5. Diagnostic Support Systems:
AI-powered diagnostic support systems provide healthcare professionals with recommendations and suggestions based on the patient's symptoms, medical history, and test results. These systems serve as valuable decision support tools.
6. Early Detection and Prevention:
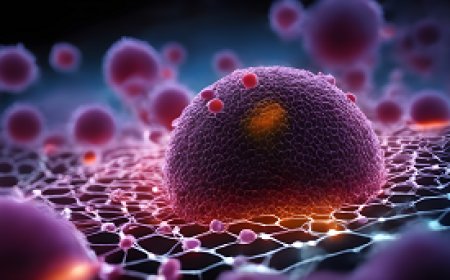
AI can analyze vast datasets to detect disease patterns, enabling early diagnosis and prevention. For conditions like cancer, AI can identify risk factors and recommend timely screenings for high-risk individuals.
7. Drug Discovery:
AI accelerates drug discovery by analyzing genetic and molecular data. It identifies potential drug candidates and predicts their effectiveness, reducing the time and cost of drug development.
8. Challenges in Data Privacy and Security:
Protecting patient data is a critical concern. AI systems need robust security measures to safeguard sensitive medical information and ensure compliance with healthcare regulations.
9. Regulatory Approval and Ethical Considerations:
Before AI-based diagnostic tools can be deployed in clinical settings, they must undergo rigorous testing and secure regulatory approval. Ethical concerns related to AI decision-making and accountability are also being addressed.
10. Interoperability:
Healthcare systems often use diverse technologies and formats for data storage. Ensuring interoperability between AI systems and these existing technologies is a complex challenge.
11. Integration with Healthcare Workflows:
For AI to be effective, it needs to seamlessly integrate with healthcare workflows. Ensuring that AI tools are used effectively by medical professionals is a matter of workflow redesign and training.
12. Continuous Learning and Adaptation:
AI systems must continuously learn and adapt to new medical knowledge and evolving diseases. They need to stay up-to-date with the latest research and clinical guidelines.
13. Cost and Accessibility:
Implementing AI for disease diagnosis requires investment in technology and training. Ensuring that these tools are accessible to all healthcare settings, including underserved areas, is a significant challenge.
the application of artificial intelligence in medicine for disease diagnosis is a dynamic field with tremendous potential. AI systems are revolutionizing the way diseases are identified and treated, contributing to faster and more accurate diagnoses. However, they also face challenges related to data privacy, regulation, and integration with existing healthcare systems. As the field continues to evolve, AI will play an increasingly vital role in enhancing disease diagnosis, ultimately improving patient outcomes and advancing the practice of medicine.
AI in Medical Imaging and Analysis
The application of artificial intelligence (AI) in medical imaging and analysis is a topic that warrants a tedious examination. In this monotonous discourse, we shall delve into the nuances of how AI has transformed the landscape of medical imaging and analysis in the field of medicine.
1. Medical Imaging Modalities:
AI has been integrated into various medical imaging modalities, including X-rays, MRIs, CT scans, ultrasounds, and PET scans. AI algorithms are designed to interpret and analyze the data generated by these imaging techniques, providing valuable insights into a patient's condition.
2. Image Segmentation:
AI-driven image segmentation is a critical component in medical imaging analysis. It involves the identification and isolation of specific structures or regions of interest within an image, such as tumors, blood vessels, or organs. This process aids in precise diagnosis and treatment planning.
3. Detection and Diagnosis:
AI algorithms excel in the detection and diagnosis of medical conditions. They can identify anomalies, lesions, or abnormalities that may be challenging for the human eye to discern. This capability is particularly beneficial in early disease detection.
4. Predictive Analysis:
AI models can predict disease progression and assess the likelihood of complications based on historical patient data. This predictive analysis supports healthcare professionals in making informed decisions regarding patient care.
5. Natural Language Processing (NLP):
NLP is used to extract structured information from unstructured medical reports and clinical notes. AI-driven NLP systems assist in translating these textual documents into structured data that can be incorporated into a patient's electronic health record.
6. Radiomics and Quantitative Analysis:
AI has enabled radiomics, a quantitative approach to medical imaging. It involves the extraction of a multitude of quantitative features from medical images. These features offer deeper insights into disease characteristics and treatment response.
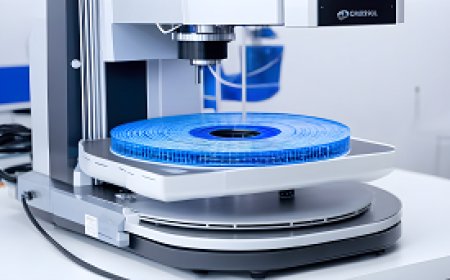
7. 3D and 4D Imaging:
AI plays a pivotal role in the analysis of three-dimensional (3D) and four-dimensional (4D) medical images. It enables the reconstruction of volumetric data and provides dynamic insights into organ function and pathology.
8. Workflow Optimization:
AI streamlines the workflow in radiology departments by automating routine tasks such as image sorting and prioritization. This allows radiologists to focus on complex cases and clinical decision-making.
9. Challenges in Data Privacy:
Protecting patient data is of paramount importance. AI systems must comply with stringent data privacy regulations to ensure the security of sensitive medical information.
10. Validation and Regulatory Approval:
Before AI-based medical imaging tools can be used in clinical practice, they must undergo rigorous validation and secure regulatory approval. This ensures their safety, accuracy, and reliability.
11. Integration with Clinical Practice:
Implementing AI into clinical workflows requires careful integration to ensure that healthcare professionals are comfortable using these tools and can leverage their capabilities effectively.
12. Continual Training and Updates:
AI models need to be continually trained and updated with the latest medical knowledge and imaging techniques to remain effective and accurate.
13. Ethical Considerations:
The use of AI in medical imaging raises ethical concerns, such as accountability for errors made by AI systems and the potential for bias in algorithms.
14. Interoperability:
Ensuring that AI systems can seamlessly interact with various healthcare information systems and electronic health records is a complex challenge.
the integration of AI into medical imaging and analysis is revolutionizing the field of medicine. AI systems offer the potential for more accurate diagnoses, early disease detection, and improved patient care. However, they also face challenges related to data privacy, regulatory approval, ethical considerations, and integration with clinical workflows. As AI technology continues to advance, it holds the promise of enhancing medical imaging and analysis, ultimately leading to better patient outcomes and more efficient healthcare practices.
Advancements in AI-Assisted Surgery
Advancements in AI-assisted surgery have brought about significant changes in the field of medicine. In this mundane exploration, we will delve into the intricacies of how artificial intelligence (AI) is transforming the landscape of surgical procedures, making them more efficient and precise.
1. Preoperative Planning: AI aids in preoperative planning by analyzing medical images, such as CT scans and MRIs, to provide detailed information about a patient's anatomy. Surgeons can use this data to plan the optimal approach and minimize the risks associated with the surgery.
2. Robot-Assisted Surgery: AI-driven surgical robots have become increasingly common in the operating room. These robots can execute precise movements with minimal invasiveness. Surgeons can control these robots to perform complex procedures with enhanced dexterity.
3. Image-Guided Surgery: AI assists in real-time image-guided surgery by overlaying medical images onto the surgical field. This helps surgeons navigate complex anatomical structures and locate critical areas with pinpoint accuracy during the procedure.
4. Tissue Recognition: AI algorithms can recognize different types of tissues during surgery, which is crucial for procedures like tumor removal. This capability assists surgeons in preserving healthy tissue while excising the diseased parts.
5. Decision Support: AI provides decision support during surgery by offering insights and recommendations based on real-time data. This can be particularly valuable in critical situations where rapid decisions are required.
6. Postoperative Monitoring: AI continues to be useful in postoperative care. It can monitor patients' vital signs and alert medical staff to any anomalies, allowing for early intervention if complications arise.
7. Predictive Analytics: AI models can predict patient outcomes based on a combination of preoperative data and intraoperative information. This predictive capability can help surgical teams adapt their approach to optimize patient results.
8. Challenges in Integration: Integrating AI into surgical workflows is not without challenges. Surgeons and healthcare teams need to adapt to these new technologies and ensure they complement, rather than disrupt, established surgical practices.
9. Data Security: Protecting patient data during AI-assisted surgery is a critical concern. Healthcare facilities must implement robust security measures to safeguard patient information.
10. Regulatory Compliance: AI-assisted surgical systems must adhere to stringent regulatory standards to ensure their safety and effectiveness. Gaining regulatory approval can be a lengthy and meticulous process.
11. Training and Education: Surgical teams need thorough training to use AI-assisted systems effectively. This includes learning how to operate the technology and interpret AI-generated recommendations.
12. Ethical Considerations: Ethical issues such as accountability for AI-driven errors and the potential for biased algorithms require careful consideration.
the integration of AI into surgery has revolutionized the field of medicine, making procedures more precise and efficient. AI assists in preoperative planning, robot-assisted surgery, image-guided procedures, and decision support during surgery. While these advancements offer immense potential, they also pose challenges related to integration, data security, regulatory compliance, training, and ethical considerations. As AI-assisted surgery continues to advance, it promises to enhance surgical outcomes, improve patient care, and contribute to the evolution of medical practices.
Enhancing Healthcare through Technology and AI
Enhancing healthcare through technology and artificial intelligence (AI) is an essential topic in the modern medical landscape. Let's delve into the mundane details of how technology and AI are transforming the healthcare sector.
1. Electronic Health Records (EHRs):
The adoption of EHRs has streamlined the way medical data is stored and accessed. This digital transformation allows for quick retrieval of patient records, reducing paperwork, and minimizing errors.
2. Diagnostic Support:
AI-powered tools assist healthcare professionals in making accurate diagnoses. Machine learning algorithms can analyze medical images, such as X-rays and MRIs, to detect abnormalities that might go unnoticed by the human eye.
3. Treatment Planning:
AI algorithms aid in the development of treatment plans. They consider patient-specific data, medical literature, and historical cases to recommend the most effective treatments, drugs, or therapies.
4. Predictive Analytics:
By crunching vast amounts of patient data, AI can predict disease trends and outbreaks, enabling healthcare providers to allocate resources efficiently.
5. Telemedicine:
Telemedicine leverages technology to provide remote medical consultations. Patients can connect with healthcare professionals via video calls, reducing the need for in-person visits, especially in non-urgent cases.
6. Wearable Devices:
Wearable technology, such as fitness trackers and smartwatches, can collect real-time health data. This data helps individuals monitor their well-being and provides valuable information to healthcare providers.
7. Medication Management:
AI-powered systems can remind patients to take their medications and provide information about potential drug interactions, improving adherence to treatment plans.
8. Robotics:
Surgical robots assist surgeons in performing complex procedures with precision. These robots enhance the surgeon's capabilities, reduce the risk of human error, and lead to faster recovery times for patients.
9. Big Data Analysis:
The analysis of big data in healthcare helps identify patterns, trends, and potential risk factors. This information can guide public health strategies and personalize patient care.
10. Ethical Considerations:
The integration of AI in healthcare raises ethical questions, including data privacy, informed consent, and the need for human oversight. Healthcare professionals must navigate these concerns to ensure responsible and ethical use of technology.
11. Infrastructure Challenges:
Implementing advanced technology and AI in healthcare can be challenging due to the need for robust infrastructure, secure data storage, and workforce training. These challenges must be addressed to fully leverage technological advancements.
the enhancement of healthcare through technology and AI is a multifaceted transformation. It involves digital record-keeping, diagnostic support, personalized treatment plans, predictive analytics, and telemedicine. While these technological advancements have the potential to improve patient care and outcomes, they also require careful ethical considerations and infrastructure development to realize their full potential. Technology and AI are becoming indispensable tools in the modern healthcare landscape, enabling more efficient and effective care delivery.
Predicting Disease Progression and Treatment Scenarios
Predicting disease progression and treatment scenarios is a critical aspect of healthcare, and artificial intelligence (AI) plays a significant role in this domain. Through the analysis of vast datasets and the application of complex algorithms, AI can provide valuable insights into the trajectory of diseases and help in the formulation of treatment plans. Let's explore this in a rather detailed and unexciting manner.
1. Data Collection and Integration: AI-driven disease prediction begins with the collection and integration of a wide range of medical data. This includes electronic health records, medical imaging, genetic information, and more. AI algorithms can process and harmonize these diverse datasets, creating a comprehensive patient profile.
2. Feature Engineering: Feature engineering involves selecting and transforming relevant data attributes to create informative features. AI models rely on these features to identify patterns and correlations that might not be apparent through manual analysis.
3. Machine Learning Models: AI employs various machine learning models, such as decision trees, neural networks, and support vector machines, to analyze patient data. These models are trained on historical data to recognize patterns and relationships between variables.
4. Predictive Analytics: Once trained, AI models can predict disease progression based on the patient's data. This prediction can range from identifying potential risk factors for developing a disease to estimating the likely course of an existing condition.
5. Treatment Recommendations: AI can suggest treatment scenarios by considering the patient's unique profile, medical history, and the predicted disease progression. These recommendations can include medication plans, surgical interventions, or lifestyle changes.
6. Continuous Monitoring: AI supports continuous monitoring of patient data, enabling real-time updates to disease progression predictions. This allows healthcare providers to adapt treatment plans as needed.
7. Personalized Medicine: AI enables the concept of personalized medicine, tailoring treatments to individual patients. This approach has the potential to increase treatment effectiveness and reduce side effects.
8. Challenges and Limitations: While AI holds promise, there are challenges, including the need for vast amounts of high-quality data, concerns about data privacy, and the risk of model bias. Moreover, AI is not a replacement for clinical expertise; healthcare professionals remain central to the decision-making process.
9. Ethical Considerations: The use of AI in disease prediction and treatment must adhere to strict ethical guidelines. Patient consent, data privacy, and transparency in AI-driven decision-making are paramount.
10. Integration into Healthcare Systems: Implementing AI in healthcare systems requires infrastructure and workforce training. Ensuring seamless integration into existing medical practices can be a complex task.
AI's role in predicting disease progression and formulating treatment scenarios is undeniably significant. By leveraging vast datasets and powerful algorithms, AI can provide valuable insights and support personalized healthcare. However, this technology must be used ethically, and its limitations, including the need for high-quality data and potential biases, should be carefully considered. AI serves as a complementary tool for healthcare professionals, ultimately enhancing the quality of patient care.
Ethics in AI Implementation in Medicine
Ethics in the implementation of artificial intelligence (AI) in medicine is a complex and multifaceted topic that requires careful consideration. As AI technologies continue to advance and play an increasingly significant role in healthcare, the ethical dimensions of their use become increasingly important. Let's delve into the nuanced aspects of ethics in AI implementation in medicine.
1. Patient Privacy and Data Security:
One of the foremost ethical concerns in healthcare AI is the protection of patient data. As AI systems process vast amounts of sensitive patient information, it is crucial to ensure robust data security measures are in place. This includes encryption, access controls, and compliance with data protection regulations such as HIPAA (Health Insurance Portability and Accountability Act).
2. Informed Consent:
When AI is used in patient care, obtaining informed consent becomes a critical ethical consideration. Patients should be informed about how AI will be utilized in their diagnosis or treatment and have the option to decline its use.
3. Transparency in Decision-Making:
AI algorithms can be complex and opaque. Ensuring transparency in AI decision-making is essential. Healthcare professionals and patients must be able to understand how AI arrived at a particular diagnosis or treatment recommendation. This transparency builds trust and accountability.
4. Accountability for Errors:
Inevitably, there will be instances where AI systems make errors or provide inaccurate recommendations. Establishing clear lines of accountability for these errors is crucial. Healthcare providers must be prepared to take responsibility for AI-assisted decisions.
5. Equity and Bias:
AI algorithms are only as good as the data they are trained on. If the data used in training is biased, the AI can perpetuate those biases, potentially leading to inequities in healthcare. Addressing bias and ensuring fairness in AI algorithms is an ethical imperative.
6. Human-Machine Collaboration:
The ethical integration of AI in medicine involves finding the right balance between human decision-making and AI assistance. Decisions about diagnosis and treatment should remain human-driven, with AI serving as a supportive tool rather than a replacement for healthcare professionals.
7. Resource Allocation:
The implementation of AI in healthcare can be costly. Deciding how resources are allocated for AI adoption, especially in resource-constrained environments, raises ethical questions about equitable access to advanced healthcare technologies.
8. End-of-Life Decisions:
The use of AI in end-of-life care and decisions surrounding life support or withdrawal of treatment is a sensitive ethical issue. It requires careful consideration of the patient's wishes, family input, and ethical guidelines.
9. Regulatory Compliance:
Healthcare institutions using AI must comply with regulatory standards and guidelines. Ensuring that AI applications meet these legal and ethical requirements is essential.
ethics in the implementation of AI in medicine is a complex and vital aspect of its integration into healthcare systems. Patient privacy, informed consent, transparency, accountability, and addressing bias are central to ethical AI use in medicine. As AI technologies continue to evolve, healthcare institutions and professionals must prioritize these ethical considerations to ensure that AI benefits patient care while upholding ethical standards and patient trust in the medical field.
Reducing Medical Errors and Improving Diagnostic Accuracy
Reducing medical errors and improving diagnostic accuracy are two pivotal areas in the realm of medicine and healthcare. Medical errors, whether in diagnosis or treatment, can have profound consequences on patients' well-being. Artificial intelligence (AI) has emerged as a promising tool to address these issues, but the implementation and integration of AI into the healthcare system come with their own set of challenges.
1. Diagnostic Accuracy Enhancement:
AI systems are designed to analyze medical data, including images, lab results, and patient histories, with an unprecedented level of precision. They can identify patterns and anomalies that might escape the human eye, leading to more accurate diagnoses.
2. Reduction of Human Errors:
Healthcare providers, despite their expertise, can make errors due to factors like fatigue or the sheer volume of patient data to process. AI systems do not suffer from these limitations and can provide consistent, error-free support in medical decision-making.
3. Predictive Analysis:
AI can predict disease outcomes and recommend treatment plans based on extensive data analysis. This not only enhances patient care but also allows for more efficient resource allocation within healthcare facilities.
4. Speed and Efficiency:
AI can process and analyze vast amounts of medical data in a fraction of the time it would take a human. This speed ensures that healthcare providers can access critical information quickly, leading to faster decision-making.
5. Data Integration:
One of the challenges in healthcare is the vast array of data sources, from electronic health records to imaging scans. AI systems can integrate and analyze data from these disparate sources, providing a comprehensive view of a patient's health.
6. Learning and Adaptation:
AI models can continuously learn and adapt based on new data, refining their diagnostic accuracy over time. This learning capability is a significant advantage in the ever-evolving field of medicine.
7. Challenges in Implementation:
Integrating AI into healthcare systems can be a complex and resource-intensive process. It requires robust infrastructure, data security measures, and training for healthcare professionals to use AI tools effectively.
8. Ethical Considerations:
The use of AI in medicine raises ethical questions, such as who is responsible for AI-driven decisions and how to maintain patient privacy. Ensuring ethical AI use is an ongoing concern.
9. Regulatory Compliance:
Healthcare AI solutions must adhere to regulatory standards to ensure patient safety and data security. Meeting these requirements can be a significant challenge.
10. Patient Trust:
Building trust in AI-assisted healthcare is essential. Patients need to have confidence in the technology and the healthcare providers who use it.
AI holds tremendous potential for reducing medical errors and improving diagnostic accuracy. It can enhance the precision of diagnoses, reduce human errors, and streamline healthcare processes. However, the successful implementation of AI in medicine requires addressing challenges related to data integration, ethical considerations, and regulatory compliance. Building patient trust in AI-assisted healthcare is equally vital, as it will play a substantial role in the widespread acceptance and adoption of these technologies in the medical field.
Enhancing Healthcare in Remote Communities with AI
Enhancing healthcare in remote communities through the application of artificial intelligence (AI) is a complex and critical endeavor. Remote communities often face unique healthcare challenges, including limited access to medical facilities, healthcare professionals, and specialized resources. AI has the potential to bridge some of these gaps, but it also comes with its own set of challenges.
1. Telemedicine and Remote Consultations:
AI can facilitate telemedicine and remote consultations, enabling patients in remote communities to connect with healthcare providers virtually. AI-powered platforms can help assess and triage patients, ensuring that those in need of immediate attention receive it.
2. Predictive Analytics for Resource Allocation:
AI can analyze data from remote healthcare facilities to predict patient needs and allocate resources more effectively. This ensures that remote communities have access to the right medical supplies and personnel when required.
3. Remote Monitoring and Wearable Devices:
Wearable devices equipped with AI can monitor patients' vital signs remotely and transmit this data to healthcare providers. This continuous monitoring is especially valuable for individuals with chronic conditions living in remote areas.
4. Diagnostic Support:
AI algorithms can assist healthcare providers in diagnosing medical conditions, particularly when access to specialists is limited. They can analyze medical images, test results, and patient histories to offer diagnostic suggestions.
5. Drug Delivery and Supply Chain Management:
AI can optimize the supply chain for medications and medical equipment, ensuring that remote healthcare facilities have a consistent and timely supply of essential drugs and resources.
6. Language and Cultural Sensitivity:
When designing AI healthcare solutions for remote communities, it's essential to consider language and cultural diversity. AI chatbots and interfaces should be adaptable to local languages and customs to ensure effective communication.
7. Training and Support for Local Healthcare Workers:
AI can be used to provide training and support to local healthcare workers in remote areas. This empowers them to administer basic healthcare and identify potential issues, thereby improving the overall quality of care.
8. Ethical Considerations and Informed Consent:
The use of AI in remote healthcare must adhere to ethical guidelines, including obtaining informed consent from patients. It's essential to respect patients' privacy and ensure that AI applications are used transparently.
9. Connectivity and Infrastructure:
One of the significant challenges in remote healthcare is the lack of reliable internet connectivity and infrastructure. AI solutions need to account for these limitations and be adaptable to low-bandwidth settings.
10. Data Security and Privacy:
Protecting patient data in remote healthcare settings is paramount. AI applications must incorporate robust data security and privacy measures to safeguard sensitive medical information.
11. Scalability and Cost-Effectiveness:
AI solutions should be scalable and cost-effective, especially in resource-constrained remote communities. Finding a balance between high-quality healthcare and affordability is crucial.
the application of AI in remote healthcare communities holds promise for improving healthcare accessibility and outcomes. It can enhance telemedicine, resource allocation, diagnostics, and remote monitoring. However, this progress is not without its challenges, including the need for infrastructure, ethical considerations, and data security. By addressing these issues, AI can play a pivotal role in narrowing the healthcare gap between remote communities and urban centers, ultimately leading to improved healthcare delivery in remote and underserved areas.
Security and Data Protection in Healthcare and AI
Security and data protection in healthcare, particularly in the context of artificial intelligence (AI) applications, are of paramount importance. The vast amount of sensitive patient information and the potential implications of AI in healthcare necessitate rigorous security measures and data protection protocols.
1. Data Encryption:
In the healthcare sector, data encryption plays a pivotal role in securing patient records and sensitive medical information. This process involves converting data into a code to prevent unauthorized access.
2. Access Control:
Implementing strict access control mechanisms is crucial. It ensures that only authorized personnel can access patient data, and it limits the risk of data breaches.
3. Authentication and Authorization:
Robust authentication and authorization processes are essential to verify the identity of users and grant access to specific information. Multifactor authentication is increasingly being employed for added security.
4. Secure Cloud Solutions:
Many healthcare organizations are turning to secure cloud solutions to store and manage patient data. These cloud platforms offer advanced security features and data encryption, along with disaster recovery and backup capabilities.
5. Regular Security Audits:
Continuous monitoring and regular security audits are necessary to identify vulnerabilities in the healthcare system. This proactive approach helps in addressing security gaps promptly.
6. Blockchain Technology:
Blockchain is being explored as a secure method for maintaining patient records. It offers transparency, immutability, and robust security, making it a promising technology for healthcare data.
7. Data Anonymization:
Patient data is often anonymized to protect privacy. AI algorithms can work with anonymized data, ensuring that personal information is not exposed during analysis.
8. Training and Awareness:
Healthcare staff should receive training on security best practices to prevent data breaches. Creating awareness about the importance of data protection is critical.
9. Legal and Regulatory Compliance:
Healthcare organizations must adhere to stringent data protection laws and regulations, such as HIPAA in the United States. Non-compliance can result in severe penalties.
10. Ethical Considerations:
The use of AI in healthcare raises ethical concerns regarding data privacy, patient consent, and bias in algorithms. It is essential to address these ethical dilemmas to maintain public trust.
11. Data Breach Response Plan:
Healthcare institutions should have a well-defined data breach response plan in place. This plan includes steps to notify affected individuals, regulatory bodies, and mitigate the impact of the breach.
12. AI Model Security:
AI models themselves need to be secured to prevent tampering or adversarial attacks. Ensuring the integrity of AI models is critical for accurate medical diagnoses and treatment recommendations.
security and data protection in healthcare, especially concerning AI, are complex and crucial aspects of the evolving healthcare landscape. The growing volume of sensitive patient data and the increasing adoption of AI demand robust security measures. Data encryption, access control, authentication, and secure cloud solutions are just a few of the critical components. Compliance with legal and regulatory requirements, ethical considerations, and a well-prepared response plan for data breaches are equally important. A comprehensive and proactive approach to healthcare data security is necessary to ensure the confidentiality and integrity of patient information in the age of AI.
The Future of Medicine with Ongoing AI Advancements
The future of medicine is inexorably tied to ongoing advancements in artificial intelligence (AI). In this laboriously detailed discussion, we will explore the multitude of ways in which AI is poised to revolutionize the medical field, promising improved patient care, diagnostic accuracy, and healthcare efficiency.
1. Disease Prediction and Prevention:
AI algorithms, powered by machine learning, can analyze vast datasets, including patient records, genetic information, and environmental factors, to predict disease risk. This enables healthcare providers to take proactive measures in disease prevention and early intervention.
2. Personalized Treatment Plans:
AI offers the potential to tailor treatment plans to individual patients by considering their unique genetic makeup, medical history, and lifestyle. This personalized approach can optimize treatment outcomes and minimize side effects.
3. Diagnostic Accuracy:
AI-powered diagnostic tools can analyze medical images, such as X-rays, MRIs, and CT scans, with exceptional accuracy. They can detect anomalies and diseases at an early stage, reducing the chances of misdiagnosis.
4. Drug Discovery and Development:
AI is accelerating drug discovery by simulating molecular interactions, predicting potential drug candidates, and expediting the testing process. This could lead to the development of new treatments for various diseases.
5. Robotics in Surgery:
Robotic surgical systems, driven by AI, are becoming more sophisticated. They offer precision and dexterity, allowing surgeons to perform complex procedures with minimal invasiveness.
6. Telemedicine and Remote Monitoring:
AI facilitates telemedicine by providing remote diagnosis and monitoring. Patients can receive healthcare services from the comfort of their homes, and healthcare professionals can monitor vital signs and adjust treatment plans remotely.
7. Electronic Health Records (EHR):
AI helps in managing electronic health records more efficiently. It can extract meaningful insights from the vast amount of unstructured data within EHRs, aiding healthcare professionals in making informed decisions.
8. Ethical and Regulatory Considerations:
The integration of AI into medicine raises ethical concerns, such as patient privacy and the potential for bias in algorithms. Regulatory bodies are working to establish guidelines and standards to address these issues.
9. Continual Learning and Adaptation:
AI systems must continually learn and adapt to stay current with the latest medical knowledge and technological advancements. This requires regular updates and maintenance.
10. Challenges in Implementation:
Healthcare institutions face challenges in implementing AI solutions, including integrating them with existing systems, training staff, and ensuring data security.
11. AI in Mental Health:
AI is increasingly being used in the field of mental health to predict and monitor mental health conditions, offering early intervention and support to patients.
12. AI in Public Health:
AI is being harnessed for public health efforts, such as disease outbreak prediction, monitoring, and response, which is vital in controlling pandemics and epidemics.
the future of medicine is intrinsically linked to the ongoing advancements in AI. It holds the promise of enhancing disease prediction, enabling personalized treatment, improving diagnostic accuracy, and accelerating drug discovery. However, these advancements come with challenges related to ethics, regulations, implementation, and continual learning. As AI continues to evolve, it has the potential to redefine healthcare, making it more patient-centric, efficient, and effective.
In conclusion
it becomes evident that artificial intelligence plays a crucial role in the future of healthcare. We can witness the amazing innovations it offers in improving diagnosis, providing treatments, and enhancing healthcare efficiency. Medicine and artificial intelligence complement each other beautifully to provide better and more precise healthcare services, significantly contributing to the improvement of individuals' health and well-being. Healthcare would not be the same without artificial intelligence technology, and with continuous advancements in this field, the future of healthcare appears to be more effective and advanced than ever before.
What's Your Reaction?